- Research
- Open access
- Published:
Using 2% PVPI topical solution for serial intravitreous injections and ocular surface findings: a case control study
International Journal of Retina and Vitreous volume 10, Article number: 41 (2024)
Abstract
Background
The use of povidone-iodine for ocular surface asepsis is widespread for intravitreal injections. They became frequent procedures, leading to serial exposure of patients’ eyes to iodinated solutions. In this study, we investigate the changes in the ocular surface in patients submitted to repeated use of povidine for intravitreal injection of anti-VEGF asepsis, analyzing Ocular Surface Disease Index, non-invasive break up time, blinking quality, lipid layer, meniscus height and osmolarity.
Methods
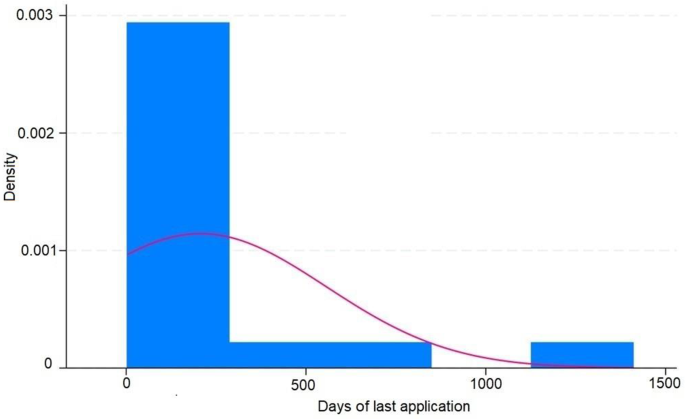
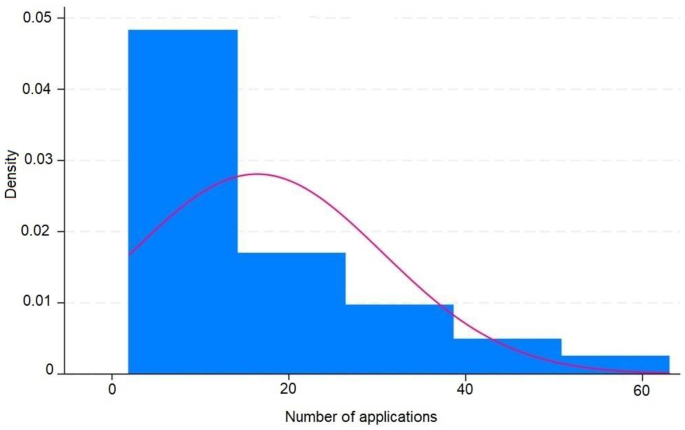
This case-control study included 34 individuals (68 eyes), 14 males, 20 females aged 48 to 94. Inclusion criteria were individuals who received application of 2% povidone-iodine eyedrops for intravitreal injections treatment with the non-treated contralateral eye used as control. Ocular surface examinations were performed at a single occasion. A pre-intravitreal injection asepsis protocol with povidone-iodine was applied. All statistical analysis was performed using the STATA® 18.0 Software and a p-value = 0.05 was considered as the statistical significance value in all tests.
Results
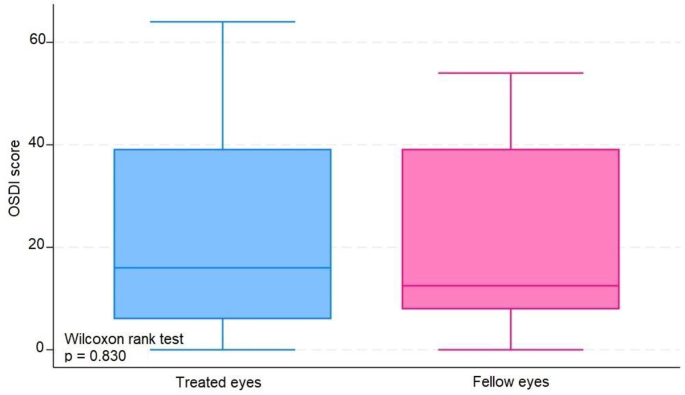
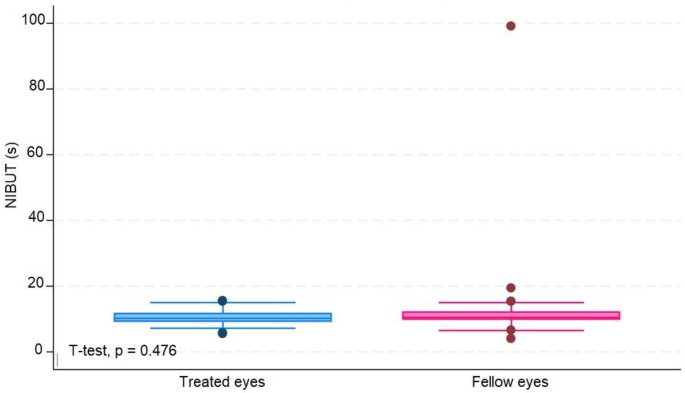
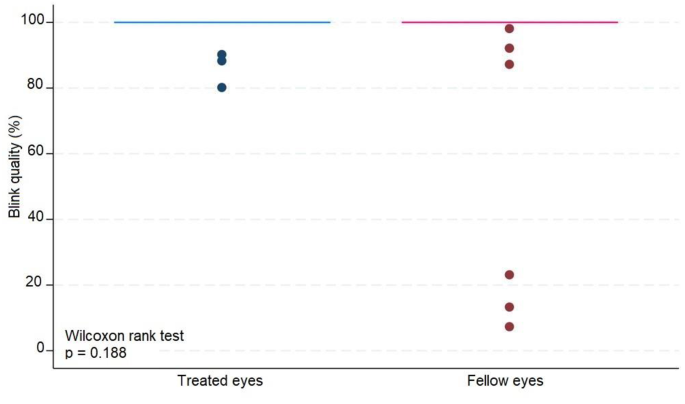
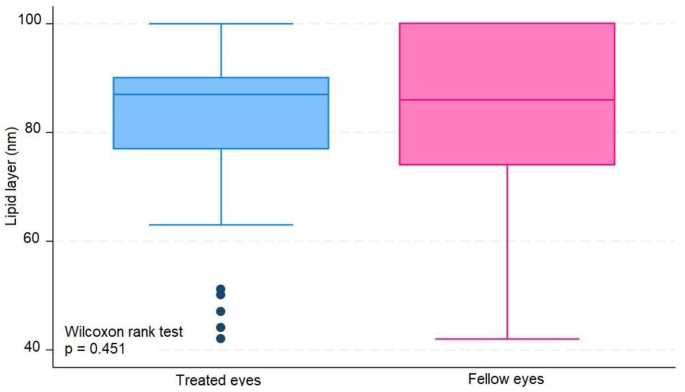
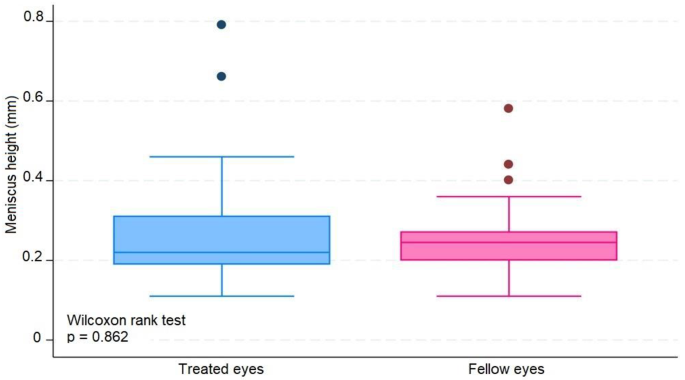
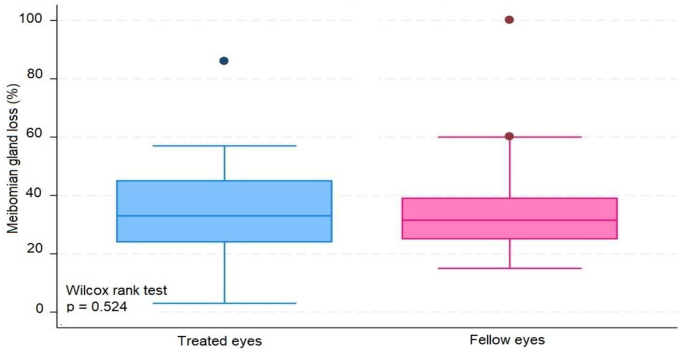
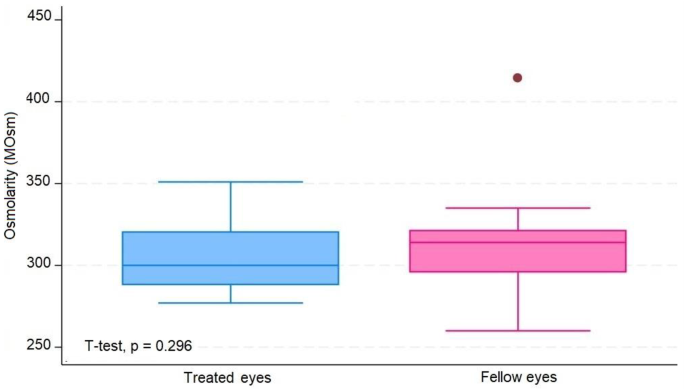
The median number of IVIs in treated eyes was 12 (range 6–20). The results in treated eyes compared with untreated eyes were respectively : median OSDI 16 (IQR 6–39) and 12.5 (IQR 8–39) (p = 0.380); mean NIBUT 10.30 (SD ± 2.62) and 10.78 (SD ± 2.92) ( s, p = 0.476); median blinking quality 100 (IQR 100) and 100 (IQR 100 ) (%, p = 0.188); median lipid layer 87 (IQR 77–90) and 86 (IQR 74–100) (nm, p = 0.451); median meniscus height 0.22 (IQR 0.19-0,31) and 0.24 (IQR 0.20–0.27) (mm, p = 0.862), median Meibomian gland atrophy 33 (IQR 24–45) and 31.5 (IQR 25–39) (%, p = 0.524); and mean osmolarity 306.6 (SD ± 21.13) and 313.8 (SD ± 29) (mOsm, p = 0.297). There was no statistically significant relationship between the repetitive use of 2% iodinated solution and signs or symptoms compatible with dry eye syndrome in this group of patients.
Conclusions
The findings suggest that 2% povidone iodine is a safe and efficacious agent for ocular surface antisepsis during intravitreal injections, not leading to substantial ocular surface modifications. This conclusion supports the continued use of povidone iodine in routine ophthalmic procedures without increased risk of inducing dry eye syndrome.
Background
The use of povidone iodine (PVPI) for ocular surface asepsis is widespread, both for surgical procedures and intravitreal injections [1,2,3,4,5]. Surgeries for cataracts, glaucoma, and intravitreal injections have become common and frequent procedures in ophthalmology, leading to the serial exposure of patients’ eyes to iodine solutions [5,6,7,8,9,10]. These changes are directly associated with dry eye syndrome [11, 12].
In particular, studies have demonstrated that intravitreal injections used to treat diabetic macular edema or age-related macular degeneration result in significant changes in the ocular surface, leading to dry eye syndrome and damage to homeostasis of the ocular surface [5, 11, 13, 14].
Dry eye syndrome is a multifactorial disease of the ocular surface characterized by the loss of tear film homeostasis, hyperosmolarity, inflammation, damage and neurosensory abnormalities [11, 15,16,17,18]. Its etiology is variable, ranging from nonspecific inflammation of the ocular surface to direct chemical or physical aggression, infections, and autoimmune diseases [11, 12, 15, 19].
In addition to the most common symptoms, burning sensation, itching, speck, eye redness, excess tearing reflex, brightness sensitivity, and quality of vision loss are also frequent findings that affect efficiency at work and the quality of life of patients [11, 12, 15, 19, 20].
This study aimed to observe changes in the ocular surface and tear film due the serial use of 2% PVPI, the gold standard drug for asepsis of the ocular surface. As it is well known that pre-injection antisepsis of the ocular surface with PVPI has a toxic effect on the corneal epithelium, the aim is to identify changes in the tear film and ocular surface and avoid serious problem like dry eye syndrome [11, 12, 21, 22].
Methods
A case-control study was conducted at the Ophthalmology and Psicology Clinic (APMTO MD) in Londrina, Paraná. The patients were recruited from the Retina and Vitreous Institute (AMBC MD) in Londrina, Paraná. The study included 34 individuals (68 eyes). 14 males, 20 females, aged 48 to 94 years. All participants signed the informed consent form, which allowed their participation in the study. Inclusion criteria were individuals who received application of 2% PVPI eyedrops for anti-VEGF IVIs treatment with the contralateral eye used as control, that had not been treated with any topical medication during the same period of applications and good comprehension of the Ocular Questionnaire Surface Disease Index (OSDI). Exclusion criteria were patients who could not understand the OSDI questionnaire; patients using antidepressant medicine, diuretics, sympathomimetics, eye drops for glaucoma, or eye lubricants; people with allergies to iodine; unfavorable clinical conditions to undergo the examination procedures for the study; inappropriate test quantity and quality; unsatisfactory images or unsatisfactory and inadequate data.
The study was approved by the Ethics and Research Committee Involving Human Beings of the State University of Londrina by N. 5.300.176.
The individuals underwent directed clinical and ophthalmological analysis, received explanations about the study, used their data, and signed consent forms. All clinical measures were performed using the IDRA equipment (SBSSISTEMI, Orbasano, Torino, Italy), at which time the OSDI questionnaire was also applied and tear osmolarity was collected using the I-PEN® (I-MED PHARMA INC. Dollard-des-Ormeaux, QC, Canada). All examinations and administration of the questionnaire were performed by the same professional. No drops or medications that could cause changes in any subsequent measurements were used.
The variables analyzed were age, sex, date of the last PVPI application, number of PVPI applications, OSDI questionnaire, tear osmolarity, NBUT, tear film interferometry, tear meniscus height, percentage of meibomian gland loss, and blink quality. The sequence of procedures obeyed the following order: Explanation to the subject regarding the exams and questionnaire to which he would be submitted, guidance to the patient not to identify in any way the eye being treated and the eye not treated during data collection, nor during the questionnaire OSDI; patient positioning in the IDRA® equipment; capture of blinking quality video images; capture of tear film interferometry; capture of images to measure the height of the tear meniscus and immediate measurement; capture of tear film (NBUT); image capture for the percentage of meibomian gland loss by everting the lower eyelid with a cotton swab; positioning the patient outside the IDRA equipment; application of the I-PEN® electrode to capture tear osmolarity in the lower conjunctiva, first in the right eye, and subsequently in the left eye; application of the OSDI questionnaire.
All statistical analyses were performed using STATA® 18.0 Software and p-values ≤ 0.05 indicated statistical significance.
The Shapiro-Wilk test was used to verify data normality. Data that did not follow a normal distribution were analyzed using the Wilcoxon rank-sum test and were described as means and as medians and interquartile ranges. Data that showed normality were analyzed using the Student’s T test and presented as means and standard deviations. Descriptive, quantitative, and multivariate analyses compared treated (case) and untreated (control) eyes.
Results
The average number of IVIs in treated eyes was 12 (range 6–20). The results in treated eyes compared with untreated eyes were respectively: median OSDI 16 (IQR 6–39) and 12.5 (IQR 8–39) (p = 0.380); mean NIBUT 10.30 (SD ± 2,62) and 10.78 (SD ± 2.92) ( s, p = 0.476); median blinking quality 100 (IQR 100) and 100 (IQR 100 ) (%, p = 0.188); median lipid layer 87 (IQR 77–90) and 86 (IQR 74–100) (nm, p = 0.451); median meniscus height 0,22 (IQR 0.19–0.31) and 0.24 (IQR 0.20–0.27) (mm, p = 0.862), median Meibomian gland athrophy 33 (IQR 24–45) and 31.5 (IQR 25–39) (%, p = 0.524); and mean osmolarity 306.6 (SD ± 21.13) and 313.8 (SD ± 29) (mOsm, p = 0.297).). The results revealed that the use of 2% PVPI did not affect the analyzed variables in a statistically significant way. All data is summarized on Table 1.
These results are disposable on fig 1, 2, 3, 4, 5, 6, 7, 8 and 9 as annexed.
Through multivariate analysis, we obtained some interesting outcomes as follows:
When controlling for NIBUT, meibomian gland atrophy, number of applications, and days of the last application according to treatment, sex was an important variable in explaining the variability in the OSDI score (coef = 15.63 | p-value = 0.003). On average, controlling for the abovementioned variables, being female contributed to an increase in the OSDI to 15.63 points.
After controlling for meniscus height and age according to treatment, tear osmolarity contributed significantly to variability in the lipid layer (coef = -0.266, p = 0.004). In this sense, the addition of one unit in tear osmolarity led to a -0.266 drop in the lipid layer.
After controlling for meniscus height, OSDI, days since the last application, age, and sex according to the treatment, these factors contributed significantly to the variability in the lipid layer [(coef = 0.562 | p-value = 0.004) (coef = − 5.622 | p-value = 0.048)]. In this sense, the addition of one year of age led to a decrease of -0.562 on average. For the same treatment group, female sex led to a decrease of -5,622.
Age, lipid layer, meniscus height, sex according to treatment, age according to treatment, and sex were important factors for explaining the variability in tear osmolarity.
We noticed that a greater age correlated with lower tear osmolarity. However, being in the treated group reduced the decrease in tear osmolarity with advancing age.
Being female implied higher tear osmolarity. However, the increase in tear osmolarity was smaller in the treated group.
A greater height of the lipid layer and meniscus correlated with lower tear osmolarity.
Discussion
The present study showed that the use of topical PVPI at 2% did not cause significant damage to the ocular surface when the findings of the ocular surface and tear film analyses were used.
Our results contradict some existing data indicating the toxicity of long-term iodine use on the ocular surface; we found two statistically relevant results that the application of iodine may improve the stability of the tear film in the elderly and women, since the eyes in older individuals and female patients that received iodine showed a smaller increase in tear osmolarity [4, 14, 23, 24].
Moreover, the results of this study corroborated some hypotheses that the use of PVPI could be positive in some dry eye disease diagnostic features, such as the improvement of the tear film meniscus height and the decrease of the tear film osmolarity [25, 26].
A localized anti-inflammatory surface effect of the anti-VEGF agent used in intravitreous injections should be considered and assessed in further studies [22, 25].
The literature review also shows that there was an improvement in the tear function of some patients who used iodine in ocular asepsis [25,26,27], perhaps due to an antimicrobial action preventing the proliferation of bacterial flora that could produce harmful enzymes or cause meibomitis and blepharitis [25, 26, 28].
The cell regeneration mechanism might have satisfactorily recomposed the ocular surface or the tear homeostasis might have compensates for the damage caused by iodine in the cells in question; furthermore, these are just hypotheses.
We also determined that the risk factors for dry eye disease, age and female sex [10, 16, 29, 30], were associated with the observed clinical data: greater ages lower the height of the tear meniscus, the greater the tear osmolarity, and the smaller the lipid layer of the tear film. The female sex was also associated with higher OSDI scores and fewer tear film lipid layers.
Regardless of the cause or consequence, the osmolarity and lipid layer of the tear film were inversely proportional.
Through multivariate analysis, we determined that the risk factors for dry eye syndrome, age, and female sex correlated with worse results in the tear meniscus measurement tests, OSDI questionnaire, and tear film interferometry, corroborating the literature implicating them as risk factors for dry eye disease [20, 30, 31].
Moreover, due to the sample size, false negatives, or simply because in practice, iodine in the amount and frequency used does not lead to histological damage that may reflect functional changes. The results did not discourage the use of iodine for ocular asepsis but also did not indicate its use for protocols with higher concentrations or more applications than those used in current protocols.
The strengths of the study are as follows: the same patient was the control and treated group, avoiding any environmental or medical bias. The number of injections administered was higher than that reported in other studies. No drops were used during the examination to avoid artificial changes to the tear film.
The limitations of this study were as follows: the study had a small sample size of 34 patients, resulting in 68 eyes being analyzed, which may have caused an analysis bias when using these data in the general population. We must remember that the analyzed population was from southern Brazil and had mostly descended from Italian, German, Spanish, and Portuguese immigrants; therefore, these data may only reflect the specific epidemiology of this population. The meibomian glands analyzed were located in the inferior tarsus.
Conclusions
The use of iodine on the ocular surface was not significantly associated with any of the evaluated parameters. There were no statistically significant correlations between the tests applied to the case eyes. The current study indicates that the application of 2% topical povidone-iodine (PVPI) does not inflict significant damage to the ocular surface, as evidenced by the analyses of the ocular surface and tear film. Notable strengths of this study include the use of the same patient as both the control and the treated subject, which minimizes potential biases from environmental or medical factors. Additionally, the absence of any artificial agents during the examination ensures that the tear film remains unaltered.
Contrary to previous concerns regarding the long-term toxicity of iodine on the ocular surface, our findings suggest potential benefits of iodine application in stabilizing the tear film, particularly in older individuals and female patients. This is supported by a smaller increase in tear osmolarity in these groups following iodine application. Furthermore, the study corroborates hypotheses that PVPI may positively affect certain Dry Eye Disease diagnostic features, such as improved tear film meniscus height and reduced tear film osmolarity.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- PVPI:
-
Povidine or polyvinylpyrrolidone-iodine
- IVIS:
-
Intravitreal injections
- VEGF:
-
Vascular endothelial growth factor
- OSDI:
-
Ocular Surface Disease Index
- NIBUT:
-
Non invasive break up time
- BQ:
-
Blink quality
- LL:
-
Lipid layer
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- NM:
-
Nanometer
- MM:
-
Miliimeter
- mOsm:
-
Miliosmol
References
Oakley C, Allen P, Hooshmand J, Vote BJT. PAIN AND ANTISEPSIS AFTER OCULAR ADMINISTRATION OF POVIDONE-IODINE VERSUS CHLORHEXIDINE. Retina. 2018;38:2064–6.
Fukuda M, Shibata S, Shibata N, Fujita N, Miyashita H, Tanimura N, et al. Polyvinyl alcohol-iodine induced corneal epithelial injury in vivo and its protection by topical rebamipide treatment. PLoS ONE. 2018;13:e0208198.
Grzybowski A, Brona P. Povidone-iodine is still a premium antiseptic measure in ocular surgery. Acta Ophthalmol. 2017;95.
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo C-K, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–83.
Craig JP, Nelson JD, Azar DT, Belmonte C, Bron AJ, Chauhan SK, et al. TFOS DEWS II Report Executive Summary. Ocul Surf. 2017;15:802–12.
Moss SE. Prevalence of and risk factors for Dry Eye Syndrome. Arch Ophthalmol. 2000;118:1264.
Jiang X, Wang Y, Lv H, Liu Y, Zhang M, Li X. Efficacy of intra-meibomian gland injection of the anti-VEGF agent bevacizumab for the treatment of meibomian gland dysfunction with lid-margin vascularity. Drug Des Devel Ther. 2018;12:1269–79.
Kim S, Ahn Y, Lee Y, Kim H. Toxicity of povidone-iodine to the ocular surface of rabbits. BMC Ophthalmol. 2020;20:359.
Malmin A, Thomseth VM, Førland PT, Khan AZ, Hetland HB, Chen X, et al. Associations between serial Intravitreal injections and Dry Eye. Ophthalmology. 2023;130:509–15.
Audelan T, Legrand M, M’Garrech M, Best A-L, Barreau E, Labetoulle M, et al. Vieillissement de la surface oculaire : physiopathologie et conséquences pratiques pour la prise en charge. J Fr Ophtalmol. 2018;41:262–70.
Kanclerz P, Myers WG. Potential substitutes for povidone-iodine in ocular surgery. Eye. 2021;35:2657–9.
Reibaldi M, Avitabile T, Bandello F, Longo A, Bonfiglio V, Russo A, et al. The effectiveness of 0.6% povidone Iodine Eye drops in reducing the Conjunctival bacterial load and needle contamination in patients undergoing Anti-VEGF intravitreal injection: a prospective, randomized study. J Clin Med. 2019;8:1031.
Han SB. Prevalence of Dry Eye Disease in an Elderly Korean Population. Arch Ophthalmol. 2011;129:633.
Silas MR, Schroeder RM, Thomson RB, Myers WG. Optimizing the antisepsis protocol: effectiveness of 3 povidone–iodine 1.0% applications versus a single application of povidone–iodine 5.0%. J Cataract Refract Surg. 2017;43:400–4.
Zhang X, Wang L, Zheng Y, Deng L, Huang X. Prevalence of dry eye disease in the elderly. Medicine. 2020;99:e22234.
Donnenfeld ED, Holland EJ, Solomon KD, Fiore J, Gobbo A, Prince J, et al. A Multicenter Randomized Controlled Fellow Eye Trial of pulse-dosed Difluprednate 0.05% Versus Prednisolone acetate 1% in cataract surgery. Am J Ophthalmol. 2011;152:609–e6171.
Grzybowski A, Kanclerz P, Myers WG. The use of povidone–iodine in ophthalmology. Curr Opin Ophthalmol. 2018;29:19–32.
Bramantyo T, Roeslani RD, Andriansjah A, Sitorus RS. The efficacy of 1% Chloramphenicol Eye Ointment Versus 2.5% povidone-iodine Ophthalmic Solution in reducing bacterial colony in Newborn Conjunctivae. Asia-Pacific J Ophthalmol. 2015;4:180–3.
Bourcier T, Acosta MC, Borderie V, Borra´s F, Gallar J, Bury T, et al. Decreased corneal sensitivity in patients with Dry Eye. Invest Opthalmology Visual Sci. 2005;46:2341.
Niederkorn JY, Kaplan HJ. Rationale for Immune Response and the Eye. Immune Response and the Eye. Basel: KARGER; 2007. pp. 1–3.
Saedon H, Nosek J, Phillips J, Narendran N, Yang YC. Ocular surface effects of repeated application of povidone iodine in patients receiving frequent intravitreal injections. Cutan Ocul Toxicol. 2017;36:343–6.
Beni´tez-del-Castillo JM, Acosta MC, Wassfi MA, Di´az-Valle D, Gegu´ndez JA, Fernandez C et al. Relation between Corneal Innervation with Confocal Microscopy and Corneal Sensitivity with Noncontact Esthesiometry in Patients with Dry Eye. Investigative Opthalmology & Visual Science. 2007;48:173.
Yu K, Asbell PA, Shtein RM, Ying G-S. Dry Eye subtypes in the Dry Eye Assessment and Management (DREAM) study: a latent Profile Analysis. Transl Vis Sci Technol. 2022;11:13.
Dohlman TH, Lertsuwanroj B, D’Amico DJ, Ciralsky JB, Kiss S. Evaluation of signs and symptoms of ocular surface disease after intravitreal injection. Acta Ophthalmol. 2019;97.
Zoukhri D. Effect of inflammation on lacrimal gland function. Exp Eye Res. 2006;82:885–98.
Shelanski HASM. PVP-iodine: history, toxicity, and therapeutic uses. J Int Coll Surg. 1956;25:727–34.
Kemeny-Beke A, Szodoray P. Ocular manifestations of rheumatic diseases. Int Ophthalmol. 2020;40:503–10.
Zamora JL. Chemical and microbiologic characteristics and toxicity of povidone-iodine solutions. Am J Surg. 1986;151:400–6.
Mantelli F, Lambiase A, Sacchetti M, Orlandi V, Rosa A, Casella P, et al. Cocaine snorting may induce ocular surface damage through corneal sensitivity impairment. Graefe’s Archive Clin Experimental Ophthalmol. 2015;253:765–72.
Bever GJ, Brodie FL, Hwang DG. Corneal Injury from Presurgical Chlorhexidine Skin Preparation. World Neurosurg. 2016;96:610.e1-610.e4.
Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, et al. TFOS DEWS II Diagnostic Methodology report. Ocul Surf. 2017;15:539–74.
Acknowledgements
APMO provided IDRA analysis, and was a contributor to design the study, revised, written and approved the manuscript. AMBC Applied intravitreal injections and provided patients for the study and was a contributor to design the study, revised, written and approved the manuscript.
Funding
No grant Money was received for this resesearch.
Author information
Authors and Affiliations
Contributions
JHC analyzed and interpreted patient data, reviewed the literature and was a major contributor to the acquisition of data, interviewed the patients, sponsored supplies, designed the study and written the manuscript. APMO provided IDRA analysis, and was a contributor to design the study, revised, written and approved the manuscript. AMBC Applied intravitreal injections and provided patients for the study and was a contributor to design the study, revised, written and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate and consent for publication
Approval for the anonymous analisys of Imaging data and medical records was obtained from the Institutional Review Board.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Casemiro, J.H., Oguido, A.P.M.T. & Casella, A.M.B. Using 2% PVPI topical solution for serial intravitreous injections and ocular surface findings: a case control study. Int J Retin Vitr 10, 41 (2024). https://doi.org/10.1186/s40942-024-00557-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40942-024-00557-1